In rare hereditary storage disorders such as the Sandhoff disease or the Tay-Sachs syndrome, the metabolic waste from accumulating gangliosides can not be disposed of properly in the nerve cells because important enzymes are missing. The consequences for the patients are serious: from restricted mobility, blindness and mental deterioration to early death. Scientists at the University of Bonn are now showing why these gangliosides also occur in patients with other storage diseases and trigger an exacerbation in them. The results will soon be presented in the "Journal of Lipid Research" and can already be read online in advance.
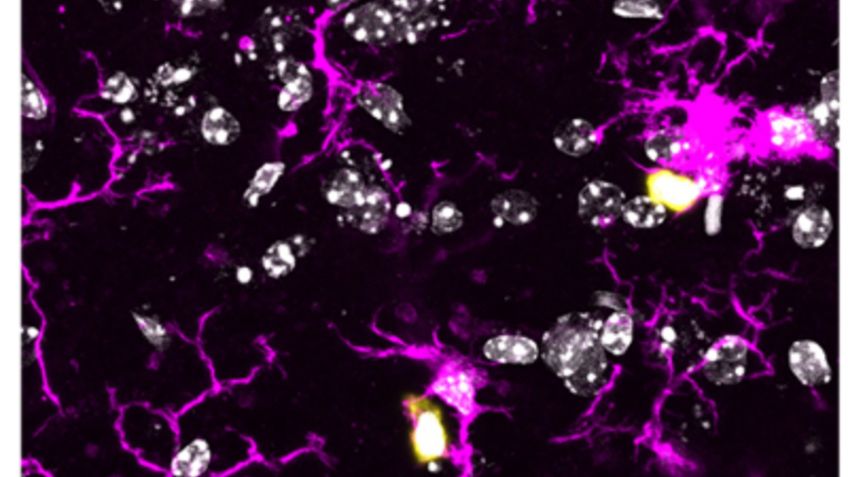
Lysosomes take over the function of the stomach in living cells. They digest superfluous metabolites and break them down into their components, which are then made available as a result of recycling for urgently needed new building materials and supplies of the cell. If the digestion in the lysosomes is blocked by, for example, genetic defects, this "cellular waste" is stored. The growing amount of waste materials can be toxic for example to nerve cells and lead to death in infancy.
In Tay-Sachs syndrome and in Sandhoff disease, components of nerve cell membranes can not be properly degraded, which is why the ganglioside GM2 is stored in the lysosomes. Gangliosides are water-insoluble fats, so-called lipids, which occur mainly in the ganglion cells of the nervous system. If, for example, the GM2-degrading enzyme Hex A is absent or impaired due to gene defects, destructive ganglioside storage occurs.
In the case of Sandhoff's disease, the degradation enzymes Hex A and Hex B are missing. As with Tay-Sachs syndrome, GM2 storage leads to the destruction of nerve cells. In the first months of life affected children develop normally, later it comes to blindness, to movement restrictions and mental deterioration - up to early death. "Previous therapeutic approaches have led to no significant success in these neurodegenerative gangliosidoses", says Prof. Dr. med. Konrad Sandhoff, Senior Professor at the LIMES Institute of the University of Bonn. Enzyme replacement therapies have failed because of the impermeability of the blood-brain barrier to these substances.
Researchers rebuild conditions in the test tube
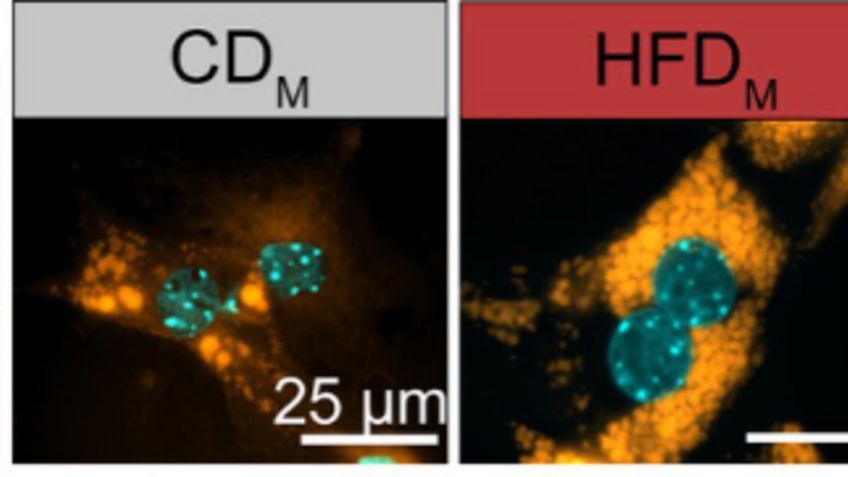
Prof. Sandhoff, together with his colleagues, Dr. Susi Anheuser and Dr. Bernadette Breiden has decoded what role the molecular environment in the lysosome plays in the successful breakdown of GM2. In the test tube, the scientists recreated the tiny bubbles (vesicles) on which the GM2 is degraded in the "cell stomach" (the lysosome). Normally, the auxiliary protein GM2AP helps to snap and release the GM2 sitting on the blister shell. Then it can be degraded to the GM3 together with the degradation enzyme Hex A. But if the function of Hex A is blocked, it will be stored with the deadly consequences for nerve cells.
The scientists used a test tube to investigate the factors that inhibit or improve the breakdown of GM2. For example, the smaller the bubbles in the "cell stomach" and the more negatively their surface is loaded, the easier the degradation enzyme can access the GM2 and the better the "digestion" function. The presence of cholesterol and sphingomyelin, however, significantly reduces GM2 degradation. Examinations revealed that in Niemann-Pick Disease precisely their storage induces additional GM2 accumulation in the lysosome, significantly worsening the type C disease, although the GM2-degrading enzyme Hex A is intact and active. "Obviously, genetic disorders of the degradation enzyme trigger a cascade of yet unknown consequential damage," Sandhoff sums up the result.
In another recent work Sandhoff's team shows that this cascade principle also applies to some hereditary mucopolysaccharidoses. One of its storage substances, the chondroitin sulfate, triggers additional ganglioside storage in the nerve cells by inhibiting GM2 degradation. In addition to existing short stature, coarsened facial features and liver enlargement, it additionally causes learning deficits and anxiety reflexes, which, however, can be alleviated again in the animal model by inhibitors of GM2 formation.
"The aim of current therapeutic approaches is to prevent the production of GM2 for these hereditary storage diseases," says Sandhoff. Medicines that have been on the market so far only partially meet this requirement. "More success promises gene replacement therapy, which has already been successful in animal models and will soon be used in patients," the biochemist continues. With the help of ferries, genes with the correct construction plan for the GM2 degradation enzyme are to be channeled into the nerve cells of the brain. Sandhoff: "Hopefully, the future will soon show if this is actually a treatment option."
Publication: Susi Anheuser, Bernadette Breiden, and Konrad Sandhoff: Membrane lipids and their degradation compounds control GM2 catabolism at intralysosomal luminal vesicles, Journal of Lipid Research, DOI: 10.1194/jlr.M092551
Contact:
Prof. Dr. Konrad Sandhoff
Seniorprofessor am LIMES-Institut
Universität Bonn
Tel. 0228/735346
E-Mail: sandhoff@uni-bonn.de
In February 2019, Prof. Konrad Sandhoff received the “Award for a Lifetime of Service to Research and Knowledge of Lysosomal Storage Diseases” by the Lysosomal Diseases New Zealand (LDNZ) for his lifelong contributions to the research on lysosomal storage diseases.











![[Translate to englisch:] [Translate to englisch:]](/fileadmin/_processed_/5/3/csm_Sandhoff_publ._Jun19_39f2c758bc.jpg)